From KERA:
As COVID-19 spreads across Texas, many physicians are turning to telehealth whenever possible. Instead of seeing patients in-person, doctors are holding appointments virtually, hoping to slow the virus’ spread by keeping people out of waiting rooms and ERs.
For doctors like primary care physician Melanie Christina in Dallas, video chatting with patients is her new normal.
After watching other parts of the U.S. struggle to meet the needs of COVID-19 patients, Christina said she’s using telehealth to responsibly practice social distancing and help prevent local hospitals from overflowing.
“In this circumstance, the people I worry most about are in the front lines — the ERs, the doctors and the hospitals,” she said. “New York City is inundated with visits and deaths. I just can’t imagine being there. Thank God for telehealth right now.”
In the midst of this outbreak, Christina said a telehealth diagnosis would be based heavily on a patient’s history, and physicians are taking extra precautions.
“We can usually tell or get a good idea how acute someone is. If we need to see them, we would bring them in for sure, so that we would not put a patient at risk for misdiagnosis,” Christina said.
“We are trying really hard to take care of our patients without having them actually come to the clinic, because the more they’re exposed to other people,” there is increased risk of infection, Bishara said.
For the first time, “patients are realizing that we can take care of them without them having to come to the clinic every time,” she said.
However, Bashira adds virtual health care has its limits.
“Medicine is really a very human thing to do. You really can’t replace the on-on-one, the eye contact, the things that you do when you’re in the same room together,” she said.
In some cases, telehealth can lead to a misdiagnosis.
When 21-year-old Verylncia Nelson got a sore throat, then had trouble swallowing, she called her insurance company to figure out the best way to get treated. This happened before the COVID-19 outbreak, and the Dallas woman said her carrier suggested seeing a doctor online, so Nelson could avoid paying out of pocket for an office visit or pricey trip to urgent care.
At first, telehealth seemed ideal.
“You just send in a picture and talk to a doctor, and they give you a prescription. So, I was like cool, that sounds fun,” Nelson said.
During the appointment, Nelson said she realized “the doctors have to take your word for it” because they have no other option.
But after receiving a diagnosis and a prescription for antibiotics, things took a turn.
“The first medication that they gave me was to treat mono. Well, the medicine ended up giving me an allergic reaction, alongside not even curing what I had, because I had strep,” she said. “My tonsils in the back of my throat had closed pretty much to a point where I couldn’t breathe, so I had to go to the emergency room.”
There are more limitations to telehealth besides misdiagnosis. Bishara acknowledged that connecting with people who aren’t able to access video technology is another.
“Our older patients tend to struggle with this. So, sometimes we co-opt some of their family members and use their phones, provided we have proper identifications so we can at least talk to them and see them,” she said.
In some cases, an old-fashioned telephone call might even work. Bishara said physicians might have to dig a little deeper to find the answers they need.
“If a patient will not be very forthcoming, it’s because they either … don’t want to hear a problem or they didn’t do something that you recommended, and they’re feeling like they don’t really want to ‘fess up. Sometimes you just have to read between the lines,” she said.
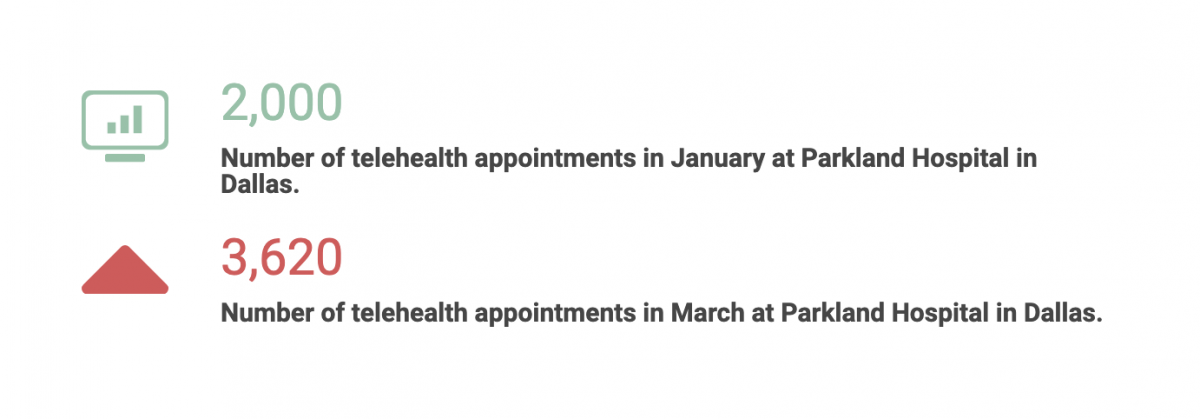
For now, people are willing to trust a new system. At Parkland Hospital in Dallas, telehealth appointments have skyrocketed.