From KUT:
Even before the COVID-19 pandemic, there was a shortage of full-time registered nurses working in health care settings. A range of issues, including long hours and strenuous working conditions, contributed to this trend. It’s a problem the state has been tracking since 2001, when the 77th Texas Legislature authorized the Nursing Workforce Reduction Program, which has pumped funding into nursing education programs across the state.
But 20 years and one pandemic later, Texas’ nursing gap is as critical as ever. During COVID-19, nurses were pushed to the point of burnout and left the profession, many taking decades of experience with them.
In 2018, the Texas Center for Nursing Workforce Studies estimated there were 27,786 fewer active registered nurses than there was demand for. The center projected that deficit would swell to more than 57,000 by 2032. The center has not released a new report since the start of the pandemic, but Texas Nurses Association CEO Serena Bumpus said she expects an updated study of the nursing workforce will yield even more troubling data.
“We have to figure out how we’re not only going to recruit more nurses into the profession, but how we’re going to retain,” Bumpus said. “You either have been touched by a nurse or you will be touched by a nurse at some point in your life. … Without nurses, our health care system will crumble.”
‘Moral distress’
Lately, Bumpus has spent a lot of time advocating for lawmakers to increase funding for nursing schools and improve working conditions for nurses. In late February, she led hundreds of nurses to the Texas Capitol, where they lobbied for bills including House Bill 112 and Senate Bill 240, which hone in on workplace violence prevention, and House Bill 901 and Senate Bill 244, which extend existing programs to recruit and fund education for potential nursing faculty.
Meanwhile, nurses who have stayed in the profession — as well as new graduates who have entered the field in the past few years — are up against difficult circumstances.
Taylor Critendon, a critical care nurse at Ascension Seton Medical Center, said she feels the absence of workplace mentors she used to rely on. Although she only had a few years of experience under her belt before COVID-19 hit, Critendon now finds herself one of the most senior nurses in her unit. She’s even served as a preceptor, or a clinical instructor for nurses in training.
“I am being looked to to help educate our brand new nurses on the floor, when we could have had folks that had been working with us for 20 years or 10 years at the bedside,” she said. “Those folks were invaluable to the entire team and to the quality of the patient care that we are able to give.”
Critendon, along with 72% of her nursing colleagues at Ascension Seton Medical Center, voted to unionize in September of last year. One of the union’s goals is to secure lower staffing ratios; Critendon said nurses in her workplace are assigned up to five or six patients at a time, which she feels is at least one too many.
“Many nurses have woken up in the middle of the night freaking about, like, ‘Oh my gosh, did I forget to give this medication?’ . . . That’s the kind of moral distress nurses take home.” she said. “But if there were more resources around, if there were extra hands and safer staffing, then nurses could actually take the time to sit down and think critically about what’s going on with their patients.”
Ascension Texas, for its part, said in a statement that it is experiencing a nursing shortage just as other health care systems throughout the country are, and that it remains committed to recruiting and retaining nurses.
Critendon has seen a lot of new nurses hired, most of them fresh off graduation from nursing school. But she said it’s difficult to keep those new hires in the profession when they are quickly overwhelmed by their workloads.
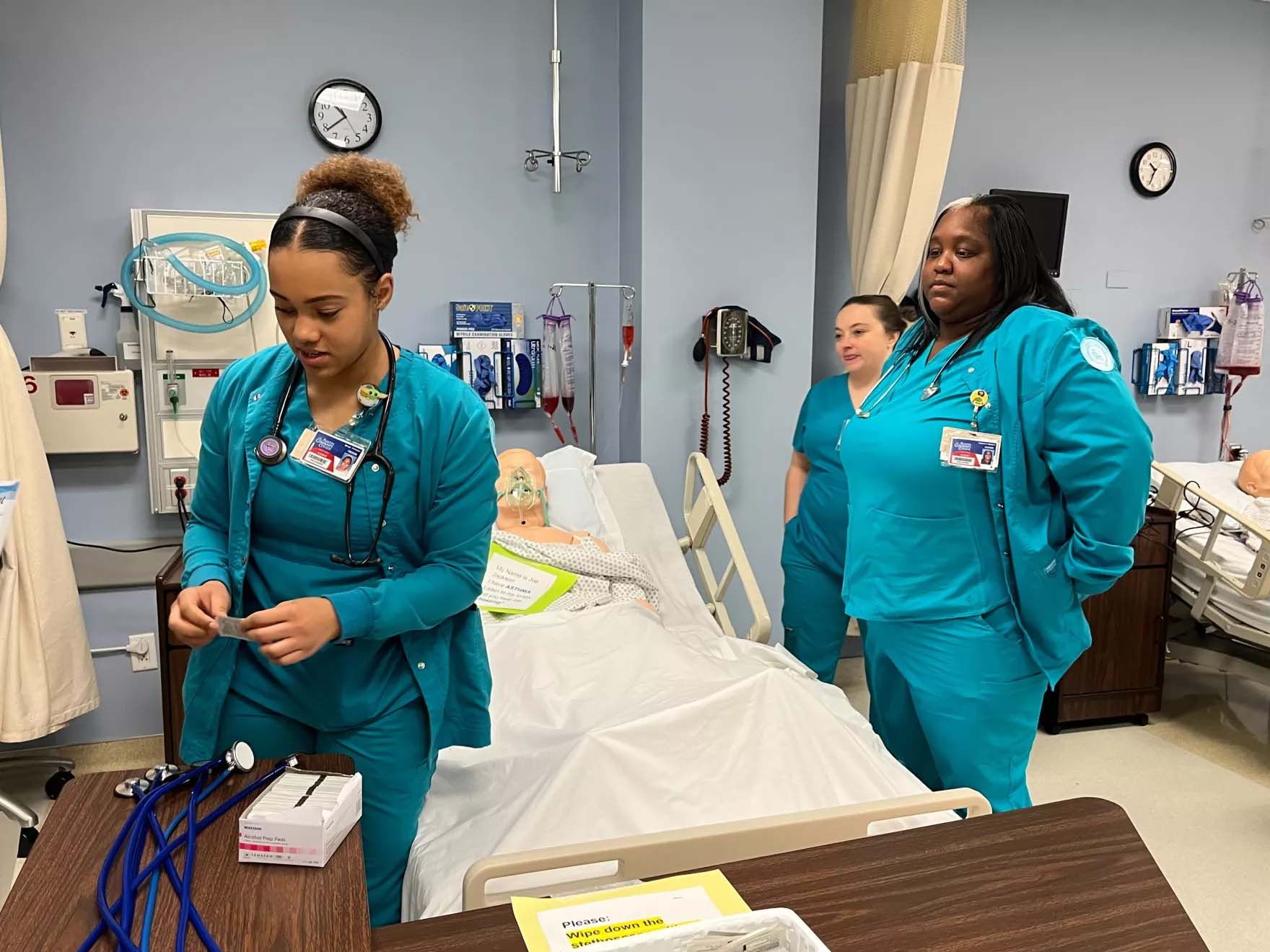
Getting students in the door
Nursing programs, meanwhile, simply can’t churn out enough graduates to keep up with demand. It’s not for a lack of qualified applicants: In 2022, the Texas Center for Nursing Workforce Studies reported 13,720 qualified applicants were denied admission to Registered Nurse training programs in Texas because there wasn’t enough space for them.
Leadership from the nursing schools at ACC and UT Austin both said they want to admit more prospective nurses, but there are two major roadblocks to doing so.
First, there is a shortage of qualified people willing to accept faculty roles in nursing programs. These positions can be a tough sell when those applicants can make more money as nurse practitioners, for instance.
Second, there are limited clinical placements available, meaning real-world medical settings where student nurses can learn hands-on skills. This issue connects back around to short staffing, as nurses in clinical settings are often too busy or too inexperienced to train others.
While local programs may not be equipped to expand their cohorts of nursing students, they are thinking creatively about how to upskill existing nurses to build the next generation of leadership in the field. For instance, UT Austin recently received a grant to support nurse preceptors by creating a clinical teaching toolkit and bootcamp for them. This could offer support to newer nurses in training roles like Critendon.
However, UT Dean of Nursing Alexa Stuifbergen said the program also serves another function.
“They like working with students so much in that preceptor role in a hospital setting that they’re very interested in becoming a faculty member, and then, hopefully, an academic career,” Stuifbergen said.
Meeting nurses where they are
ACC is similarly looking at how to best use their resources to build nurses’ skills by meeting them where they are. In the past year, ACC launched an online option for RNs to earn a Bachelor of Science in Nursing. That degree prepares RNs for more leadership opportunities and a broader range of roles in the field.
“One of the things that we wanted to be very conscientious of was needing to make our programs available to working nurses and to meet and adjust sometimes to their very challenging work schedules,” said John Nation, a professor in ACC’s RN-to-BSN program.
One of Nation’s students, Ellen Spann, said this online structure has enabled her to move to the next level in her career while still working full-time in the medical surgical unit of St. David’s South Austin Medical Center — and taking care of her 4-year-old son as a single mom.
“It’s so beneficial in that I’m still giving back to the nursing community, and I’m still giving back to the patient population — while continuing my education,” she said.
Spann said she’s committed to the nursing profession, despite its challenges. She wants to build on her current experience, learning more about surgical and post-operative nursing. If she can find opportunities to learn that fit with her responsibilities as a working parent, she doesn’t see any limits.
“It would be amazing if I could get my nurse practitioner’s [license] and set up my own clinic, having other nurses work under me,” she said. “I’m sure after being in education for a few years and having my son start school, that might not be a reality. But I certainly have the drive and desire.”