From Texas Public Radio:
In April, health officials in Houston issued an urgent notice about rising cases of congenital syphilis, imploring pregnant women to get tested and treated for a condition that can kill or debilitate infants. New county data showed it had caused at least 14 fetal deaths in 2020, marking a 250% increase over the year before.
Congenital syphilis, which occurs when the sexually transmitted disease is passed from woman to fetus and is avoidable if caught and treated in time, had been steadily ticking upward in the city, tracking rising syphilis infections among women. More babies are born with the condition in the Houston area than anywhere else in Texas, which has the nation’s highest rate of congenital syphilis.
“Nobody’s making a big enough deal about this,” said Dr. Irene Stafford, an OB-GYN and maternal-fetal medicine specialist in Houston. “What will it take? Where is the funding, where are the big media campaigns? …We have babies dying from something 100% preventable, so where is the big response?”
Statewide, 528 cases of congenital syphilis were reported to the Texas Department of State Health Services in 2019 — the latest data available — up from 367 in 2018, when Texas accounted for more than a quarter of cases nationwide. The state’s congenital syphilis rate — the number of cases per 100,000 live births — ranked worst in the country for two years running and is far above the national average. More than 80% of Texas cases have been reported in Houston, Dallas, San Antonio and surrounding areas.
Data provided to Public Health Watch via an open-records request show that between 2016 and 2019, most Texas babies with congenital syphilis were born to Black and Hispanic women, including almost nine of every 10 cases in 2018. In the Houston area, every baby who died from congenital syphilis in the last two years was either Black or Hispanic.
In emails, the state health department said it was addressing the problem by educating physicians and patients and improving data reporting and collection. It pointed to enhanced surveillance and better capacity to identify congenital syphilis as reasons for Texas’ worst-in-the-nation ranking. But the agency’s own 2021 report said the state is experiencing “true increases in both syphilis and congenital syphilis cases.”
Many factors are likely colliding to drive up syphilis among Texas women – and, in turn, congenital syphilis, experts say. Among them are inadequate sexual health education, rising addiction, lack of access to family planning services and chronically underfunded STD prevention programs. The condition’s early detection and treatment also hinge on larger inequities, such as who has health insurance and timely access to care. (Texas has the country’s worst uninsured rate, and the latest data show about one in four Texas women of reproductive age have no health coverage.)
On top of all this, COVID-19 forced local health departments to reassign STD investigators to pandemic control. The specialists find people who may have been exposed and ultimately break chains of disease transmission.
More babies born with syphilis also reflect gaps in the state’s safety net and missed opportunities in clinical settings. In a study published last year, researchers at the Centers for Disease Control and Prevention examined about 1,300 cases of congenital syphilis reported nationwide in 2018. More than half of the cases came from the South, including Texas. The most commonly missed opportunities in the region were lack of timely prenatal care and failure to provide proper treatment for women diagnosed with syphilis during pregnancy.

Dr. Irene Stafford
Stafford, an OB-GYN with McGovern Medical School at UT Health Houston who practices in high-risk hospitals, said she sees a pregnant patient with syphilis at least once every couple of weeks, and about two or three babies born with congenital syphilis each month.
“For every baby born with syphilis, there’s probably three more women who had it who were treated,” she said. “That’s what’s so frustrating — this is completely treatable.”
Stafford suspects future data will confirm the pandemic worsened the problem.
About 40% of babies born to women with untreated syphilis are stillborn or die as newborns, according to the CDC. Babies with the disease can also experience bone and liver problems, severe anemia and vision and hearing loss. Stafford said research on long-term impacts of treated and untreated congenital syphilis is sparse and unclear. But the real-world effects she sees are unmistakable.
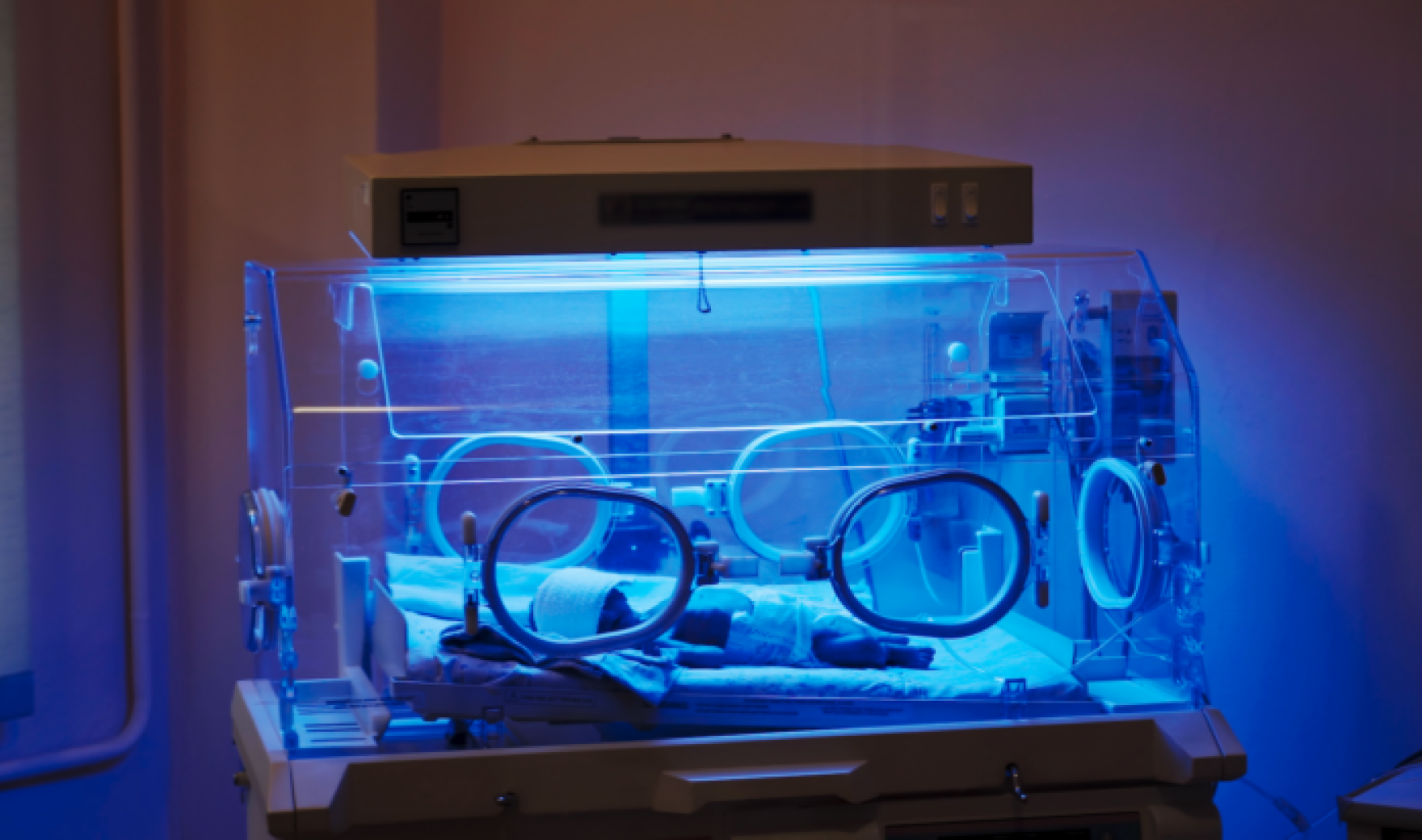
She told the story of one patient, a woman dealing with drug addiction and homelessness, who had given birth to two babies with congenital syphilis. Each time, she left the hospital before doctors could treat her, Stafford said. The older child, now 2, is in therapy for developmental delays. The younger one, born earlier this month, required treatment in a neonatal intensive care unit.
“The toll it’s taken on her family,” Stafford said. “That’s the stuff we have to think about, too — the impact this disease has on babies who do survive and their caregivers.”
Most pregnant women do seek care, she said, but still face obstacles to follow-up testing and treatment regimens.
“Many patients can’t find transportation or child care, or can’t afford to pay to park (at a hospital),” Stafford said. “We can’t just sit here and blame patients — they need our help.”
STD Rates Worsened by COVID-19

Virginia Bowen
Texas ranks worst for congenital syphilis, but national rates aren’t going in the right direction, either. In an article published in September in the New England Journal of Medicine, CDC researchers reported 2,022 cases of congenital syphilis as of July 29, 2021, surpassing the total number of cases for 2019 and reaching the highest case count since 1994.
Virginia Bowen, an epidemiologist in the CDC’s division of STD prevention, said Texas sits at the intersection of two regional trends. One is in the West, where research finds significant overlap between syphilis among women and methamphetamine use. The other is in the Southeast, where Bowen said syphilis has been historically endemic, so any sexually active person has a greater chance of contracting it, as they would gonorrhea or chlamydia, the rates of which are also soaring nationwide. “There’s a good chance that maybe Texas is experiencing a blending of these two stories,” she said. “But you’ve got to follow the local data.”
Syphilis is a reportable disease, and local public health workers are supposed to follow up with each newly diagnosed patient, Bowen said. But COVID-19 caused big disruptions to those kinds of follow-up services and the fieldwork of finding people possibly exposed to syphilis, as STD interventionists were redeployed en masse to emergency pandemic containment.
In Fort Worth, Tarrant County Public Health has made a number of changes in response to higher STD rates, including rising congenital syphilis, said Dr. Kenton Murthy, assistant medical director and deputy local health authority. Pre-pandemic, the agency switched from an appointment-only model at its STD clinics to a mix of appointments and walk-ins, increasing the number of patients who could be seen by up to 30%. It also reinforced lines of communication between its disease intervention specialists and one of the city’s main emergency rooms, where many syphilis cases are first diagnosed. Between 2016 and 2019, 68 cases of congenital syphilis were reported in Tarrant County, according to data obtained by Public Health Watch.

Vinny Taneja
Vinny Taneja, the county’s public health director, said funding for STD prevention has been relatively stagnant despite rising costs and needs. More money will help, Taneja said, but it will go only so far without parallel work to reduce barriers to the health care system.
“COVID-19 really shed a light on that part of the problem — that certain groups had worse COVID-19 outcomes compared to others due to gaps in our health care system,” Murthy said. “But STDs were already reflecting that.”
According to the National Coalition of STD Directors, the spending power of STD programs decreased by more than 40% between 2003 and 2019. At the same time, STDs have been surging, with U.S. cases of congenital syphilis nearly quadrupling between 2015 and 2019, according to CDC data. Jennifer Mahn, director of clinical and sexual health at the coalition, said STD prevention is poised to get an infusion of money — $1.13 billion in American Rescue Plan funds to hire thousands more disease intervention specialists at the local level.
“It’s just starting to get into people’s hands and implementation needs time,” Mahn said of the new funds. “I think it’s going to be a rough next year or so, but maybe in the next two or three years, we can start to move the needle on this.”
Texas lawmakers did take up rising congenital syphilis rates in 2019, passing legislation requiring physicians to test pregnant women for syphilis three times: at the first prenatal visit, during the third trimester and at delivery. But it’s unlikely all physicians are following the rules or are even aware of them, said Dr. Judy Levison, an OB-GYN in Houston and a professor at Baylor College of Medicine.
Levison co-leads a fetal and infant morbidity review board in Houston that reviews local cases of perinatal HIV and congenital syphilis to look for new trends and ways to intervene. The Houston board was launched as a pilot in 2015; similar boards were created in Dallas and San Antonio over the next few years.
Case reviews have revealed gaps in physician knowledge regarding syphilis testing and treatment during pregnancy, Levison said. In response, she said, the board hopes to persuade state Medicaid insurers to educate their providers.

Dr. Kim Onufrak
“Probably the biggest thing we’ve learned,” said fellow OB-GYN Stafford, a member of the Houston review board, “is that nobody is immune to syphilis.”
In Nueces County, congenital syphilis was already rising pre-pandemic, and COVID-19 made it worse by further restricting access to care, said Dr. Kim Onufrak, clinical director for the Corpus Christi-Nueces County Public Health District. The agency had to close its own STD clinic, which provided free or low-cost syphilis testing, to in-person visits in spring 2020 following a redeployment of staff, though it maintained tracing and treatment services. The clinic is scheduled to reopen next month.
In 2020, Nueces County reported 50 congenital syphilis cases; as of this month, the 2021 caseload was at 49. Onufrak said a majority of congenital syphilis cases in her jurisdiction occur among women without access to prenatal care or who received care very late in their pregnancies. Most low-income pregnant women are eligible for Texas Medicaid, but even then, many physicians don’t take Medicaid insurance, Onufrak said.
In South Texas, Bexar County has the state’s second-highest number of congenital syphilis cases. Preliminary data show four stillbirths related to the condition in 2020 and five so far in 2021, said Dr. Anita Kurian, assistant director at the San Antonio Metro Health District. Despite the state’s screening law, she said, about half of the county’s congenital syphilis cases are among women who do get prenatal care but don’t get treated or tested for syphilis in a timely manner.
Kurian said the health district’s community-based STD and HIV screenings are back after being suspended because of COVID-19, with multiple testing events each week, many at high-risk sites such as homeless shelters and methadone clinics. The events are picking up on more cases of syphilis among women, she said, and the data is being used to identify future testing locations.
“Rising rates of congenital syphilis are extremely disconcerting,” Kurian said. “Even asymptomatic children at birth can develop symptoms later in life.”

Lupita Thorton
Last year, facing spikes in congenital syphilis and related stillbirths, the Houston Health Department announced My Prenatal Promise, an effort to educate local women about the importance of syphilis screening during pregnancy.
Lupita Thornton, a public health investigator and manager in the department’s Bureau of HIV/STD and Viral Hepatitis, said it’s the agency’s first major STD- prevention marketing campaign.
Thornton said the department depends solely on state and CDC funds for its STD and HIV work, getting none from the city. The new federal relief funds tapped for hiring disease intervention specialists could be a game-changer, she said. But it’s also just one piece of the solution, as a baby born with syphilis is often the result of systemic breakdowns and other health and social ills.
“We need to pour money into things like mental health and drug abuse,” she said.
Several months ago, Thornton received a report about a 17-year-old girl who tested positive for syphilis. She went searching to offer her treatment, starting with family members, who said she struggled with mental health issues and ran away a lot. (“Or maybe they kicked her out because they were unable to manage her mental health issues,” Thornton said.)
Thornton found a phone number for a potential contact, who eventually gave her the best street corner and time of day to find the girl. She and her team lingered across the street, looking for someone matching her description.
They found her sitting under a bush surrounded by men, one of whom noticed the caseworkers and approached them aggressively. There was no way to safely get the girl out in that moment, and Thornton and her team were forced to retreat, losing her to follow-up.
Kim Krisberg is a contributing writer based in Austin. Blaine Young is a University of Texas journalism student and intern for Public Health Watch.