From KERA News:
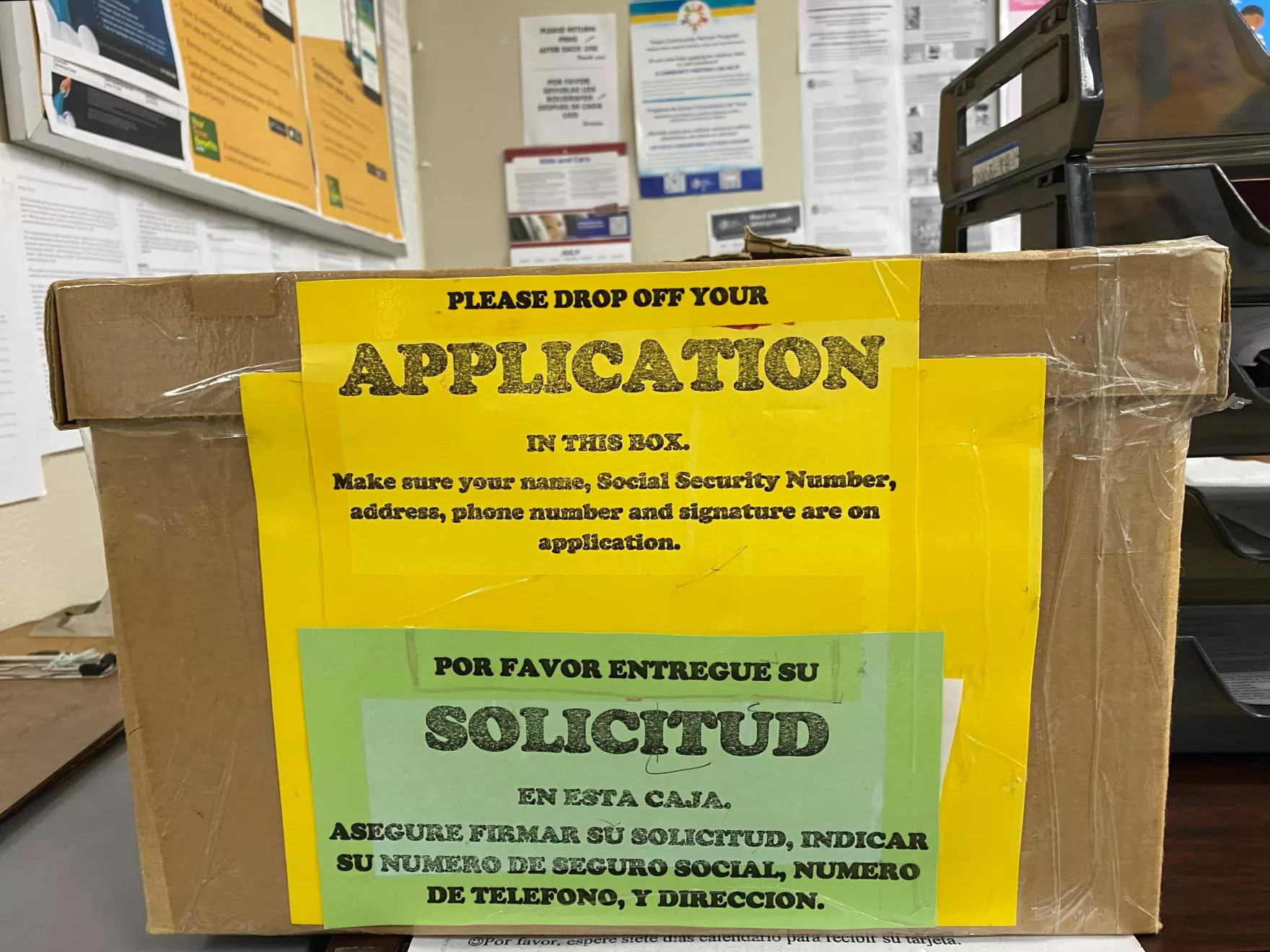
Ethel Ruano reapplied for Medicaid coverage in May, something she didn’t have to do for three years.
When officials declared the COVID-19 pandemic a public health emergency in March 2020, initiatives were put into motion to relieve struggling Americans. The Families First Coronavirus Response Act banned states from taking people off Medicaid during the pandemic, regardless of their eligibility status.
Ruano said she earns $360 to $400 each week cleaning houses part-time in Fort Worth. Her family includes her husband and three children. Her youngest, who is 16, was on Medicaid during the pandemic but now he must be reevaluated for coverage.
The enrollments for Texas Medicaid increased by 1.6 million people during the first month of the Act’s operation, an increase of 41%. Three years later, over 5.9 million Texans are enrolled in Medicaid. That’s 2 million more than at the beginning of the pandemic.
Now that the pandemic is no longer considered a public health emergency, eligibility is reverting to what it was before, and states are being forced to remove those no longer eligible.
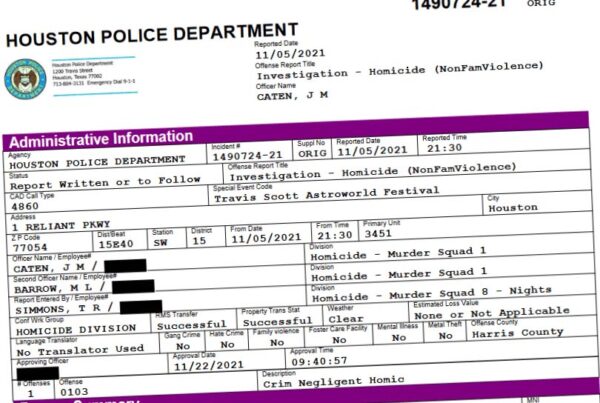
It is estimated that 50,000 people will lose Medicaid coverage in Dallas County, 15,000 in Denton County, 18,000 in Collin County, and 50,000 in Tarrant County.
“Of course, I am worried. My son has asthma. He needed psychological assistance, too,” Ruano said in Spanish.