Doctors have struggled to help patients with long haul COVID-19. Now, a team at UT’s Dell Medical School has created a program designed to help those whose symptoms don’t go away, even after weeks or months.
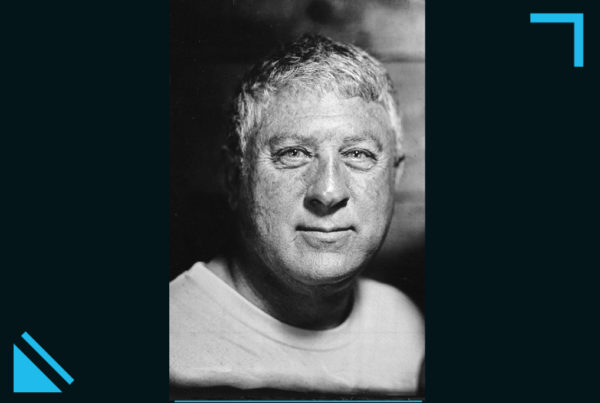
Dr. Michael Brode is the medical director of the post-COVID-19 program at UT Health Austin. He says doctors aren’t certain why some COVID-19 patients experience long haul systems, or even what percentage of those who get the virus will have extended effects. The project seeks to understand the cause, or at least, give relief to those who are suffering.
Listen to the interview above or read the transcript below to learn more about how doctors are working to help those with long haul COVID.
This transcript has been edited lightly for clarity:
Texas Standard: What is happening with these COVID long haulers? Is it known why the symptoms seem to fade and then suddenly roar back, or perhaps never go away at all?
Dr. Michael Brode: We’re just at the beginning of understanding what the underlying cause of this [is]. We’ve seen it in other viral illnesses before. After the Spanish influenza of 1918, [many] people [had] long term symptoms – neurologic problems, change in their personality. And so it may not be unique to COVID itself. We’ve just never seen it on this scale before. And there may be something specific to COVID that makes this worse, and it being a more severe virus.
Is there anything special or common among the COVID long haulers?
I really think about it in three groups of people. The problem with the research is it kind of lumps them all into one category. And I think we’ve got to get to a point where we see that, instead of talking about long COVID as a forest, we should really talk about the specific trees. And so there are three groups that I think about. One is the people who had severe illness, were in the hospital and in the ICU and they have damage and scarring from severe COVID. Another group is just people who are having persistent problems. It’s taking sometimes months for them to get over the illness. And then the third group, and I think the most troubling or difficult to talk about, is people having new symptoms after COVID in a dysregulated immune response, or almost autoimmunity following the COVID illness.
As I understand it, the new program that you and your colleagues have set up at Dell Medical Center has both a clinical and a research component.
We’re expecting that about 10 to 30% of people who have COVID will develop long COVID symptoms. And so we have a mission of being an educational resource, of making sure all doctors are comfortable taking care of these patients. We’re going to be utilizing the University of Texas to be on the front lines of understanding this disease and of course, we’re going to take care of these patients.
How many people seem be COVID long haulers?
That’s the tough part. Some estimates are up to 75% of people. But the best literature says maybe about 10 to 30%. I think that’s about right. So that’s a still a huge amount of people with the virus happening on this scale.
Some who have experienced this have deep fears that they may never feel “normal” again. What are you seeing and hearing when it comes to these ongoing symptoms?
I think in the first group, the people who have lung damage or scarring from the virus – we have good therapies that are evidence based and previously known to treat this. I think those that have dysregulated immune system are a little bit tougher. They are slowly getting better over time. And we know in other viral illnesses, people really start to get better at about a year, but it can sometimes take two to five years. We are seeing that people are getting better, but we really need to find research and therapies to speed up that process.
Is there anything that has surprised you in this process when it comes to what you’ve seen in the patients?
It’s been surprising just how prominent the neurologic disorders are. People describe having a brain fog and in one study have lost an average of seven IQ points. And almost everyone really has severe fatigue and what we call post exertional malaise – meaning they do an activity that shouldn’t be that strenuous and they feel wiped out after it.
Some people experience COVID one way, and they see the COVID long haulers and wonder, “is this real?” Are you encountering that sort of sense of disbelief about whether or not there really is this phenomenon going on?
Yes, absolutely. Patients who come in have sometimes seen four or five doctors and not gotten good answers. As a medical community, when faced with the unknown, we don’t have a good definition or even a diagnostic test of long COVID. And so sometimes our first thing to do is to downplay those symptoms, especially given our history with women and people of color. But what these patients are going through is absolutely real. And we have to believe them and take their issues seriously, even if we can’t immediately explain them from what we know.