From KERA News:
Editor’s note: This story has been updated to reflect the latest data from the Texas Health and Human Services Commission.
During the COVID-19 pandemic, the federal government put protections in place to make sure people could access health care, like testing, treatment, and doctors’ visits.
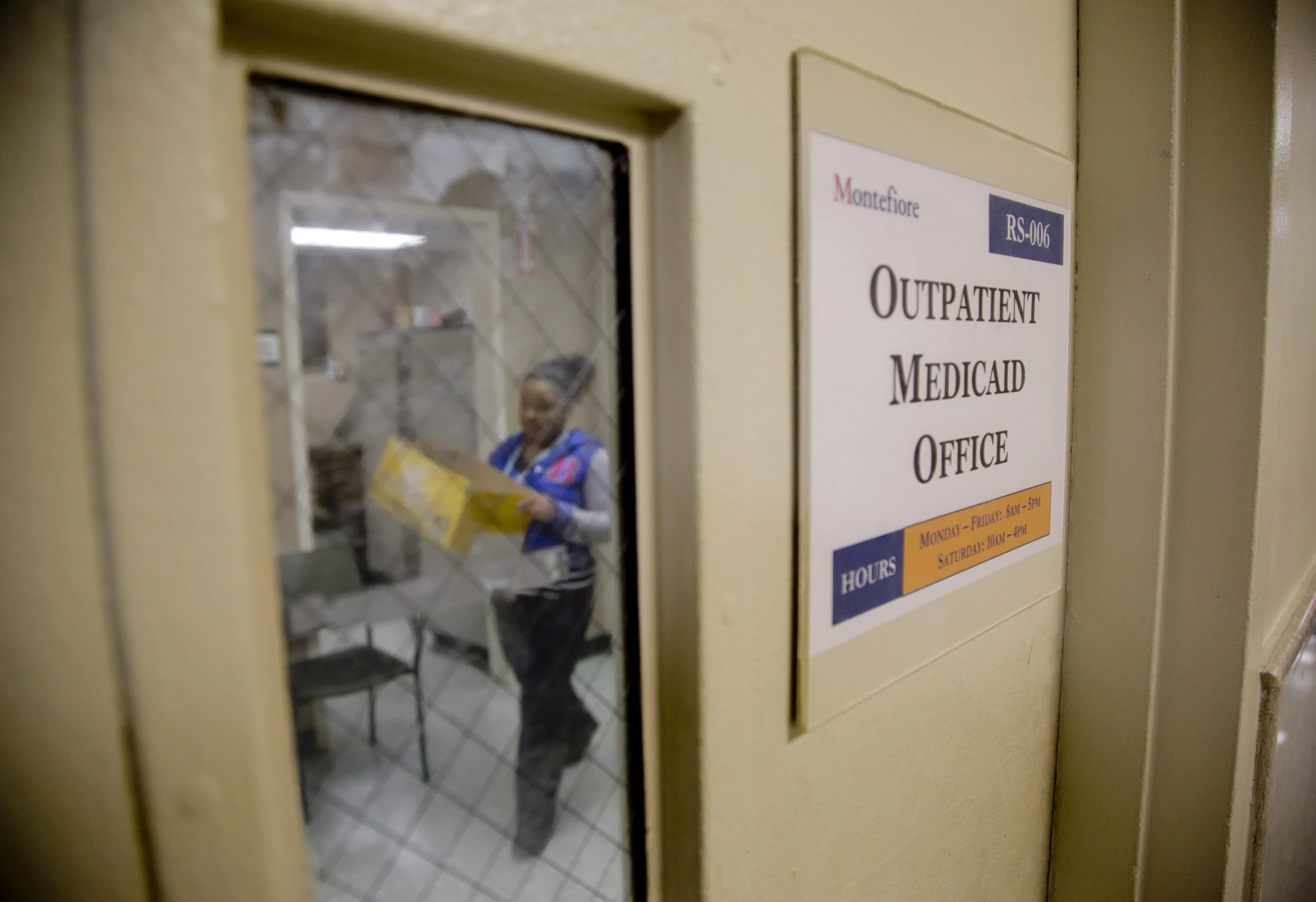
These protections under the Public Health Emergency (PHE) started in March 2020. The PHE also ensured people would have continuous Medicaid coverage, a comprehensive federal program that covers low-income people without having to reapply.
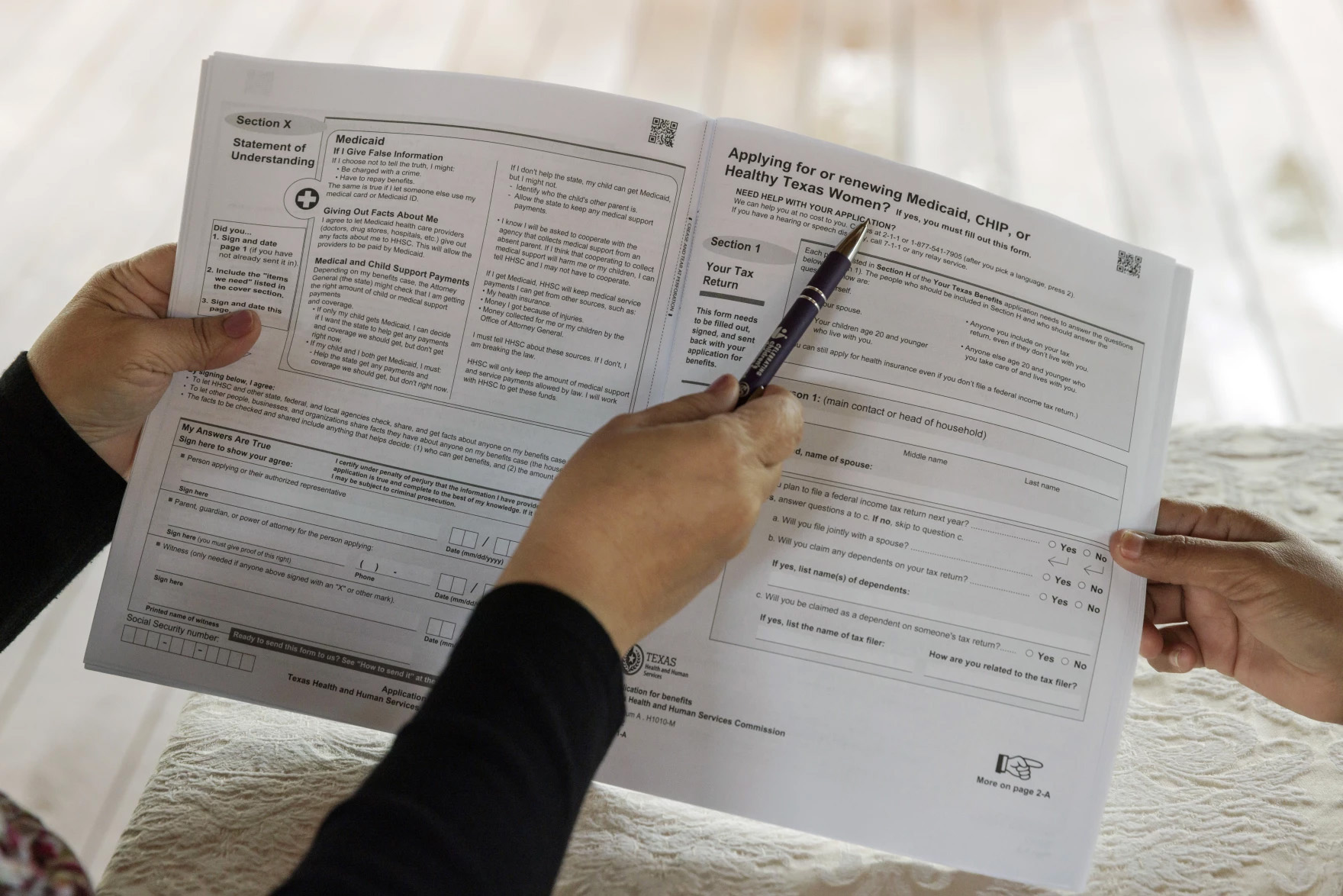
The PHE expired earlier this year. This meant that starting on April 1, states had to determine whether the millions of people who had been added to the Medicaid rolls in the past three years were still eligible.
The Texas Health and Human Services Commission (HHSC) manages Medicaid for the state and is overseeing this process. Since redetermination began earlier this year, about 1.7 million Texans have lost coverage—almost a million of them kids, according to KFF, a health policy nonprofit..
Stacey Pogue is the senior policy analyst with the advocacy group Every Texan and has been tracking Medicaid unwinding in the state. She said since a lot of folks have never renewed before, they’re running into a lot of issues, and the stakes are high.
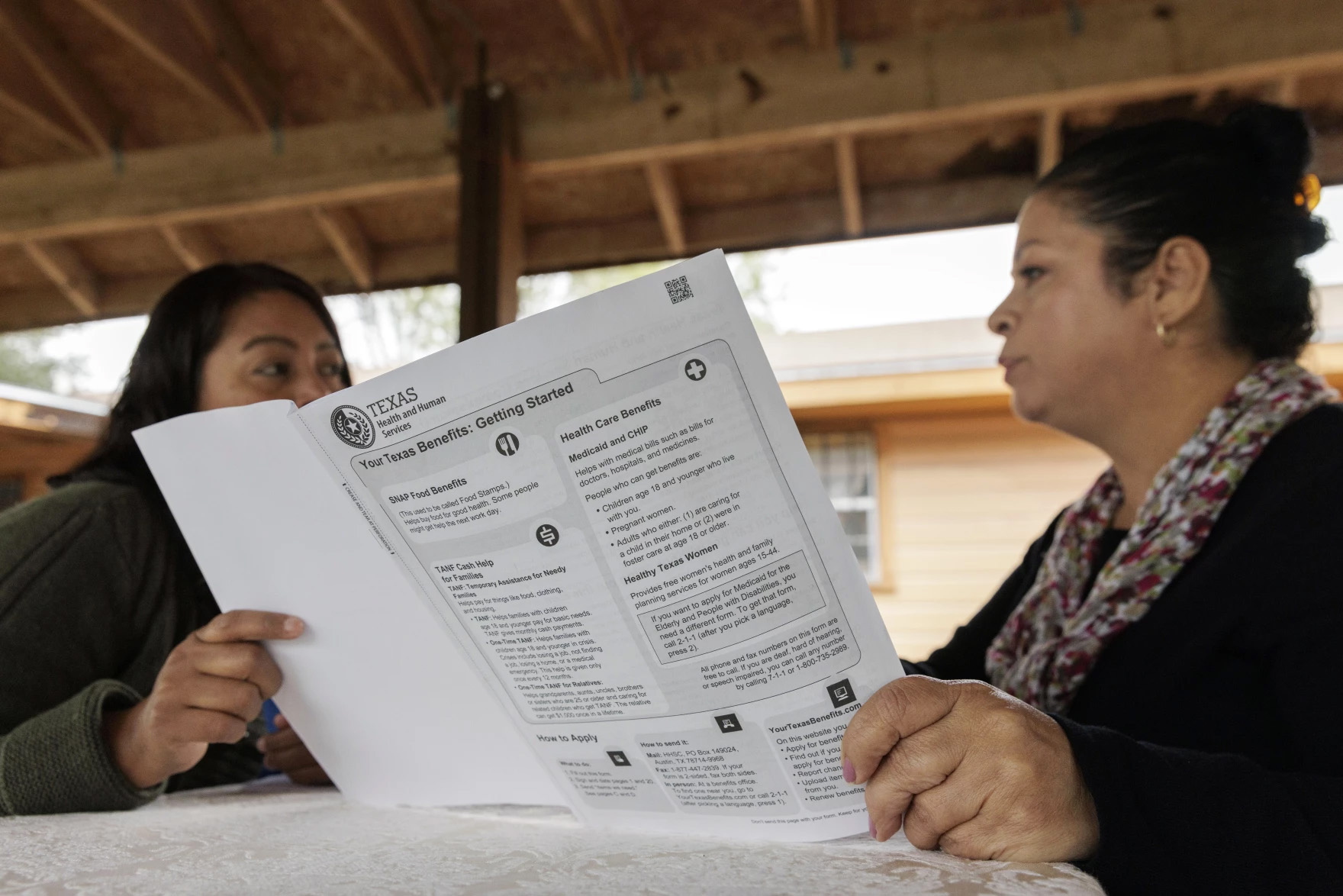
“Did the state send it to the wrong address?” said Pogue. “Did the notice come in your language? Do you understand it? Are the due dates on it clear? Can you get local help if you need it?
“We have a lot of parents who are trying to jump over every barrier in the system, and sometimes it’s just too hard with too many pitfalls for some parents to make it through.”