Click here for an audio transcript of the Texas Standard’s interview with Texas Tribune reporter Neelam Bohra on deaf children in state foster care.
From The Texas Tribune:
In early 2019, a small group of foster parents clustered in the governor’s office, hoping months of working with the state would improve things for children like theirs: deaf or hard of hearing and traumatized by a system that struggled to care for them.
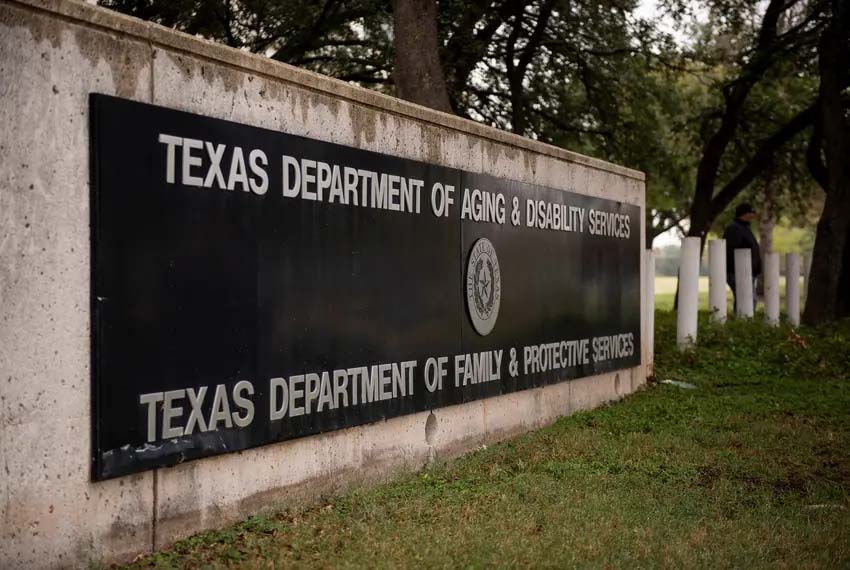
In prior meetings held between these foster parents, the governor’s office and state agencies, leaders from Texas’ Department of Family and Protective Services waffled on their methods of tracking deaf children in foster care and the number currently in the system. After foster children came forward and shared stories of abuse and neglect amplified by an inability to communicate with anyone around them, DFPS promised to give the issue more attention.
At this January 2019 meeting, state agency officials said DFPS would, on a one-time basis, check medical providers’ information to verify the number of deaf kids in the system and look for communication barriers in homes where deaf kids were placed. DFPS also said it would train staff on deafness. But the foster parents left without feeling like these were long-term solutions.
“During that meeting, I tried to remain hopeful that they would recognize and see how bad it was,” said Andrea Bright-Fontana, who lives in Austin, has fostered four deaf children and three hearing children, and is fluent in American Sign Language.
“But I felt we were blown off. I felt as though our kids didn’t matter,” she added. “And when we walked out, it felt like all of us foster parents gave up and were like, ‘I’m done.’”
More than four years later, in the wake of a pandemic, massive staff turnover and few follow-up meetings, DFPS has made little progress for deaf youth in foster care. As a result, advocates say these children are undercounted, have few ways to communicate with caseworkers and are often placed in homes that don’t use American Sign Language or understand deafness, which can stunt their social and emotional development. Deaf children who need higher levels of care are sent out of state because Texas has few behavioral health facilities accessible to deaf children.
Despite these problems, DFPS indicated it would not implement reforms recommended by the Governor’s Committee on People with Disabilities for this population of kids as recently as June, citing the “limited” size of the population as a reason for not dedicating more resources to it, according to a DFPS report from June 1.
Specifically, the governor’s committee recommended that DFPS designate an expert on deafness who has fluent sign language skills and could be an advocate for this population of children.
Jessica, whose last name is being withheld for safety concerns, is one of Bright-Fontana’s adopted foster children and said she had to beg her caseworkers to find her a foster family that uses ASL. Jessica, now 20, said she could barely make the request because there were no interpreters around in the evening hours as she sat in Child Protective Services offices. She said she mainly communicated with them by writing messages back and forth with pen and paper.
“It doesn’t matter how small the number is, it’s kids,” Jessica said. “We’re talking about kids here. All kids should have the same treatment and access.”
Tracking deaf youth
Approximately 7,000 children are deaf or hard of hearing across the state of Texas, according to statistics from the Texas School for the Deaf Foundation.
There are currently 86 deaf or hard-of-hearing children out of the more than 18,000 in the state’s custody, and only four primarily use ASL, according to the same DFPS report. But that number doesn’t come from children’s health care providers; it comes from caseworkers’ “initial assessments” based on information they get from adults who are around the child, DFPS spokesperson Marissa Gonzalez said.
When children are removed from a home because of suspected abuse or neglect, they are supposed to have at least two different medical exams within 30 days. All of them receive Medicaid health insurance through the state’s contractor, Superior Star Health. But DFPS has not worked with Superior to “identify youth with hearing impairments” according to the agency’s own June report. Superior did not respond to emails or calls asking for comment.
“The state should have insight into that [medical information] to be able to get a better accounting of it,” said Meredith Parekh, an attorney at Disability Rights Texas, a disability advocacy nonprofit.
Collecting information about these children can be hard. Caseworkers have to use IMPACT, a 1990s-era software application that state lawmakers, DFPS employees and even federal judges criticize yearly for its shortcomings. State caseworkers often have to physically track down documents missing from the system.
Jennifer Hampton, 44, previously worked as a DFPS caseworker in 2014 and was assigned to one case with multiple deaf siblings. She said the only reason she knew about their deafness, along with other health conditions they had, was because their biological parents had passed that information on to her.
“That’s all we had to go off of,” Hampton said. “We didn’t have any type of doctor’s records that said anything else.”
Translating needs
Many deaf children are nonverbal and can’t explain their situations or conditions on their own. Instead, they may rely on ASL interpreters to convey feelings to their caseworkers or other DFPS employees while in the state’s custody.
But the process of getting these interpreters is difficult. State workers can use local interpreters through an interagency contract with the Texas Health and Human Services Commission which “allows DFPS to use HHSC sign language providers for any need, including visits with children in foster care or interviews with clients during investigations,” Gonzalez, the DFPS spokesperson, said.
But Bright-Fontana recalls multiple times DFPS caseworkers didn’t bring interpreters. In one instance, her deaf foster son hit his head while running around and playing in the front yard. Foster parents have to report all of a child’s injuries to DFPS, and caseworkers will follow up to investigate the situation.
On the phone with a caseworker, she said she told them to bring an ASL interpreter. When one didn’t show up once they arrived at Bright-Fontana’s home, she said the caseworker asked Bright-Fontana herself to interpret her son’s words about what happened.
“When we got done, I turned to her and I said, ‘You do realize I could have pushed him?’” Bright-Fontana said. “I could have pushed him, I could have hurt him and you would have been none the wiser because I just interpreted between the two of you and you allowed that to happen. I told you to bring an interpreter and you didn’t.”
Kristen Schwall-Hoyt, another ASL-fluent foster parent of deaf children living in Austin, said her now adopted daughter was living with foster parents with little knowledge of Deaf culture at age 4 when they took her in for cochlear implant surgery, but no interpreters explained what was happening before or after surgery.
During such surgery, doctors place a “small, complex electronic device that can help to provide a sense of sound to a person” under the skin behind one’s ear for those who are deaf. It does not restore hearing but can help someone understand speech.
The girl told her that she woke up in pain in the hospital and tried to tell someone, including the foster parents, but no one could understand her.
“I cried and cried and cried,” said Schwall-Hoyt’s daughter, now 20, whose name is being withheld for safety concerns. “I didn’t understand a whole lot.”
Even for those who don’t primarily use ASL, it’s an important method of communication with other people, which plays a large part in a child’s development as they grow, said Wyatte Hall, an assistant professor at the University of Rochester Medical Center who has has researched clinical psychology and mental health among deaf people.
Hall said deaf children who haven’t learned ASL or don’t interact with deaf adults experience a form of trauma that stems from lack of communication, which can become so bad that they never quite understand what it means to have a conversation or use language.
Exposure to other deaf and hard-of-hearing people for deaf children is crucial to helping them grow, Hall said.
“If you don’t ever meet an adult who is deaf, how do you visualize yourself navigating the world as a deaf individual in the future?” Hall said.
Child-placing agencies, which are hired by the state to locate foster homes for abused and neglected children, are required to “make every effort to place a child with foster parent(s) who can communicate with the child” and, if they are unable, they must document any “plan to meet the communication needs of the child,” according to the Texas Administrative Code. But DFPS does not ensure agencies do this — instead, HHSC monitors their compliance, Gonzalez said.
HHSC, however, “does not track” the number or locations of any foster homes that use ASL, according to spokesperson José Araiza. Several child placement agencies did not respond to email and phone call requests for comments for this story.
“They’re already going through all kinds of traumatic experiences,” said Randi Turner, who used to serve on the Governor’s Committee on People with Disabilities. “To be placed into a setting where there’s no communication access just adds to the trauma.”
For children dependent on a higher level of care, such as that given in a residential treatment facility for behavioral health, Texas has limited options for where they can go. At least five kids in the last decade have been sent out of the state of Texas to facilities that specialize in the care of deaf children, said Parekh, the Disability Rights Texas attorney.
“We have basically created a system where, if you are a deaf child who does not have a family who is able to care for you and your behaviors in the home, you are essentially guaranteed to be placed out of state,” Parekh said.
Through the grapevine
In Austin, the deaf community is tight-knit, and many foster parents with knowledge of deafness — growing up with deaf parents themselves, working as interpreters or teachers at the Texas School for the Deaf and viewing deafness as a culture rather than a disability — became connected as they navigated the foster system.
Schwall-Hoyt and Bright-Fontana met through their shared experiences and have heard about deaf foster children through word of mouth; someone would post something on the Facebook group Texas Foster & Adoptive Parents about a deaf child, and Bright-Fontana would reach out or send over resources.
Schwall-Hoyt still receives messages from other parents or caseworkers trying to find homes for deaf foster youth. Both of them have decided to stop fostering children, but they still try to pass information around when they can.
The biggest problem is looking at deafness and ASL as if it’s a simple language barrier for kids — when it is actually a separate culture altogether, said Bright-Fontana, who trains ASL interpreters.
“You have kids that are further neglected because they’re being placed in homes that aren’t equipped to care for them and meet their needs,” Bright-Fontana said. “A deaf child is a lot of work because you have to constantly give them the language — otherwise, they don’t get language.”
Neelam Bohra is a disability reporting fellow, covering accessibility issues affecting Texans. She was a member of the 2022-23 New York Times Fellowship class. Her fellowship is a partnership between The New York Times, The Texas Tribune and the National Center on Disability and Journalism at Arizona State University. The fellowship is funded through a grant from the Ford Foundation.