From KERA News:
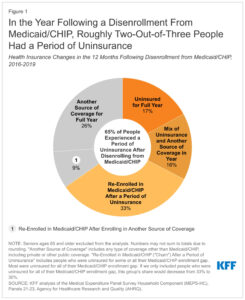
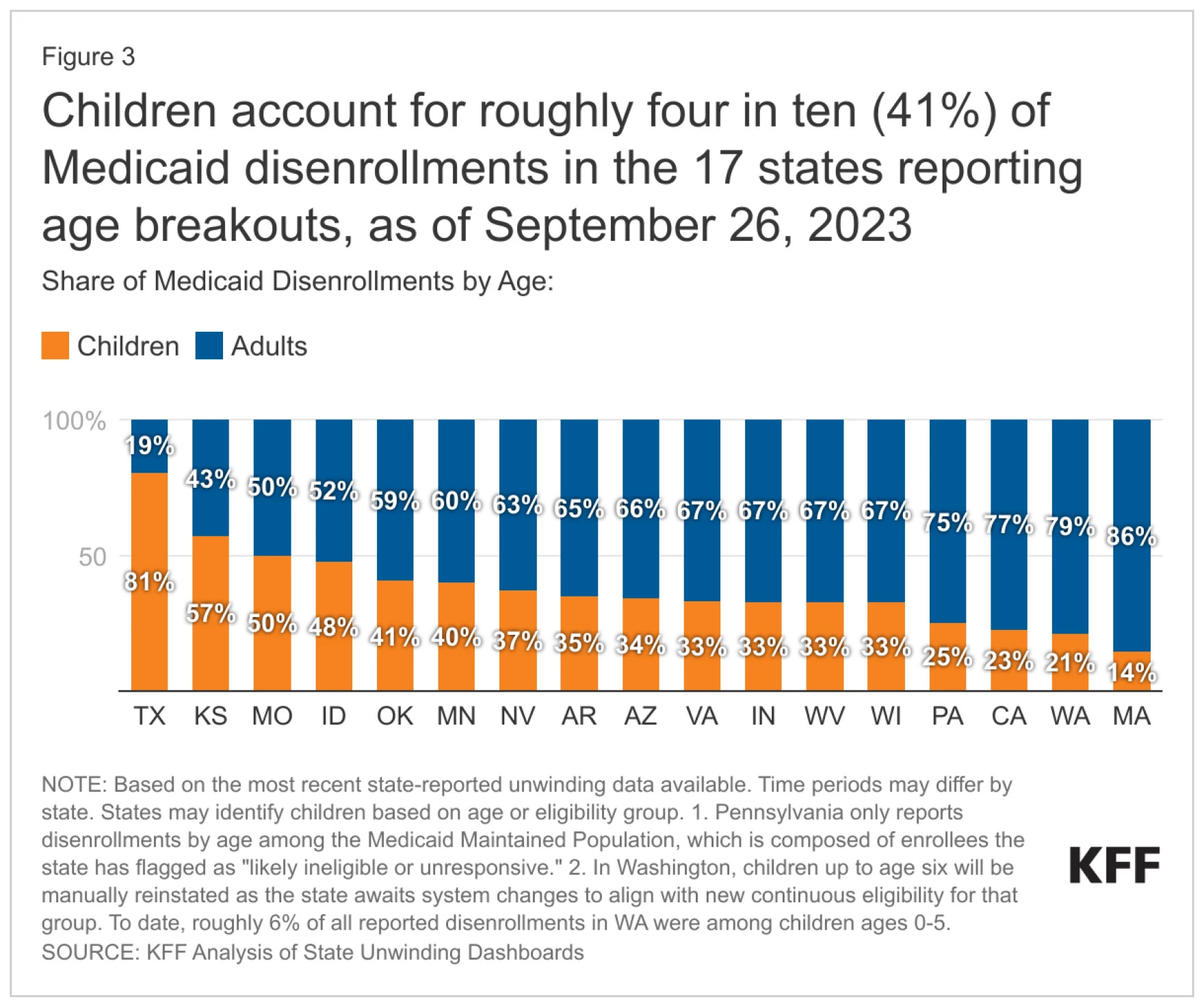
Since pandemic-era protections for health care coverage ended in March, more than 900,000 Texans have lost Medicaid coverage. For the first time in three years, many families and kids are caught up in the state’s re-enrollment process, a multi-step system of complex paperwork, deadlines and financial requirements.
Now, whistleblowers who say they work in the Texas Health and Human Services Commission (HHSC) are alleging people have been denied coverage in error because of mismanagement within the agency.